Designing behavior change and abuse mitigation for direct-care staff supporting vulnerable adults with developmental disabilities.
View Live Project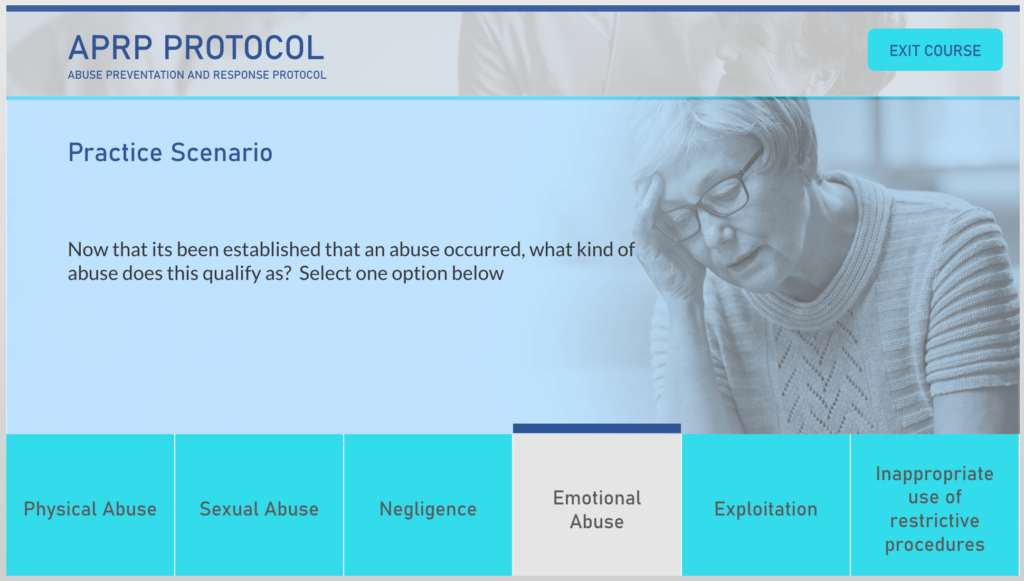
Overview
A provincial disability services agency provides state-funded supports to adults with developmental disabilities in residential care homes and community settings. These individuals—often isolated from external oversight, dependent on paid staff for daily care, and historically taught to defer to authority—are at disproportionate risk of abuse, neglect, and exploitation.
The project, titled "Recognize. Report. Respond." aimed to equip 200-500 direct-care staff, caregivers, supervisors, and administrators with the knowledge and skills to prevent, recognize, and respond to abuse in all its forms.
The Challenge
This was not a simple knowledge-transfer problem. The training had to shift staff mindsets from viewing abuse as overt (stranger danger, visible injuries) to recognizing subtle, systemic forms of harm occurring within trusted relationships.
Performance Gap Analysis:
Current State:
Desired State:
Audience Challenges:
My Approach
I applied the ADDIE framework integrated with Merrill's First Principles, Bloom's Revised Taxonomy (targeting behavioral change at "Apply" and "Analyze" levels), Kirkpatrick's Four Levels of Evaluation, and Social Cognitive Theory to address psychological barriers to behavior change.
Conducted stakeholder interviews with care home directors, frontline staff, and program officers. Performed task analysis to decompose critical responsibilities: recognize 6 abuse categories, follow reporting chain, apply prevention strategies, participate in review process. Identified psychological barriers: fear of job loss, blame culture, inadequate documentation time.
Designed assessment-first with 12 questions spanning three domains: recognition (40%), reporting & response (35%), prevention & system thinking (25%). Applied Social Cognitive Theory to address self-efficacy ("Can I recognize abuse?"), outcome expectations (reporting leads to positive impact), and environmental influences (organizational commitment, peer support).
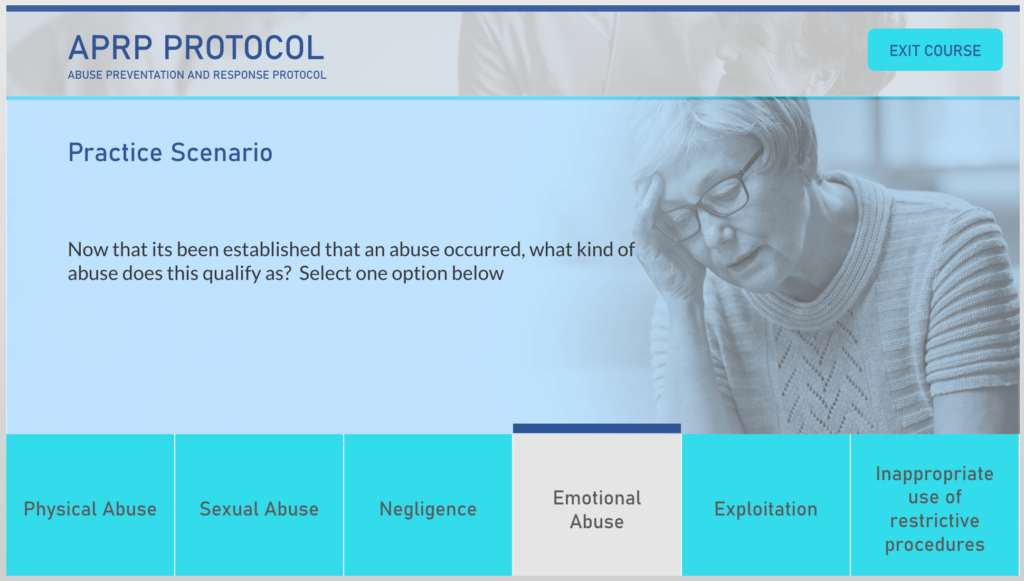
Built in Articulate Storyline 360 with 4 branching scenarios representing different abuse types: emotional abuse, neglect, exploitation, and sexual abuse/inappropriate restriction. Each scenario included decision points with consequence-based feedback showing impact on residents. Created testimonial video with real staff member (not actor) to normalize learning journey and reduce shame barriers.
Ensured WCAG 2.1 AA compliance with captions, transcripts, keyboard navigation, and screen reader compatibility. Developed 2-sided laminated staff reference card as performance support tool. Planned 4-week rollout: pilot with 30 staff, gather feedback, revise, then full deployment to 200-500 staff with manager support toolkit.
The Solution
I designed a 5-module interactive course (18-22 minutes total) that positioned abuse prevention not as a compliance burden but as fundamental to professional identity:
Module 1: Why This Matters—Vulnerability & Your Role (5 min)
Module 2: Recognize—6 Categories of Abuse (5 min)
Module 3: Report—The Protocol & Your Role (4 min)
Module 4: Prevent—Systemic Approaches to Reducing Vulnerability (4 min)
Module 5: Assessment & Commitment (3 min)
"I've worked here 12 years. When I first started, I didn't recognize the signs. A resident who was really withdrawn, wouldn't make eye contact—I just thought that was her personality. But then... I realized she was being emotionally abused by another staff member. I wish I'd known what to look for. Now I do."
Design Decisions
Three key design decisions shaped the effectiveness of this training:
Rather than framing abuse prevention as a mandatory requirement, I positioned it as fundamental to professional identity and care advocacy. The testimonial video hook established that "protecting residents matters"—appealing to staff's genuine care rather than obligation. This increased intrinsic motivation and reduced resistance.
Traditional "right/wrong" feedback wouldn't overcome psychological barriers (fear of retaliation, blame-shifting). Each scenario showed narrative consequences—seeing the resident's withdrawal deepen when abuse is ignored creates emotional encoding. Scenarios acknowledged real barriers ("I'm worried I'll lose my job") and showed how to navigate them.
Module 4 deliberately shifted focus from "What do I do when abuse happens?" to "How do we prevent abuse from happening?" This addressed root causes (power imbalances, isolation, understaffing) rather than just reactive protocols. Staff learned they could reduce vulnerability through daily practices like power-sharing and community inclusion—not just incident reporting.
Impact
Success was measured using the Kirkpatrick model to track reaction, learning, behavior, and business results:
Level 1: Reaction (Learner Satisfaction & Confidence)
Level 2: Learning (Knowledge & Skill Acquisition)
Level 3: Behavior (On-the-Job Application & Reporting)
Level 4: Results (Business Impact & Safeguarding Outcomes)
Reflection
This project reinforced that effective behavior change training must address psychological barriers, not just knowledge gaps. Staff knew abuse was wrong, but fear of retaliation, organizational loyalty, and blame culture prevented reporting. The testimonial video, policy clarifications, and consequence-based scenarios addressed these emotional barriers in ways that traditional lecture-based content never could.
The values-aligned framing was critical. By positioning abuse prevention as professional identity ("I'm part of protecting her") rather than compliance obligation, I tapped into intrinsic motivation. Staff who care deeply about residents responded to this framing far better than fear-based or rule-based messaging.
If I were to iterate, I'd conduct earlier field testing of the reference card with direct-care staff to ensure it truly functions as point-of-need support in high-stress care moments. Testing protocol lookup speed, clarity under pressure, and placement preferences would have strengthened the performance support bridge from training to real-world application.